Page 1 - Adult overactive bladder
P. 1
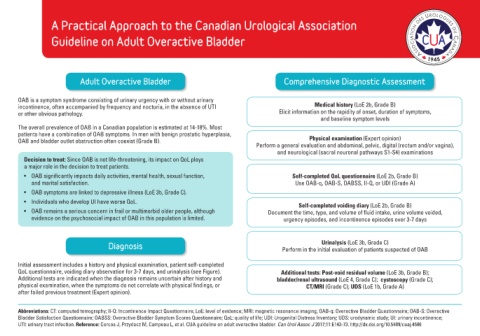
A Practical Approach to the Canadian Urological Association
Guideline on Adult Overactive Bladder
Adult Overactive Bladder Comprehensive Diagnostic Assessment
OAB is a symptom syndrome consisting of urinary urgency with or without urinary
incontinence, often accompanied by frequency and nocturia, in the absence of UTI Medical history (LoE 2b, Grade B)
or other obvious pathology. Elicit information on the rapidity of onset, duration of symptoms,
and baseline symptom levels
The overall prevalence of OAB in a Canadian population is estimated at 14-18%. Most
patients have a combination of OAB symptoms. In men with benign prostatic hyperplasia,
OAB and bladder outlet obstruction often coexist (Grade B). Physical examination (Expert opinion)
Perform a general evaluation and abdominal, pelvic, digital (rectum and/or vagina),
and neurological (sacral neuronal pathways S1-S4) examinations
Decision to treat: Since OAB is not life-threatening, its impact on QoL plays
a major role in the decision to treat patients.
• OAB significantly impacts daily activities, mental health, sexual function, Self-completed QoL questionnaire (LoE 2b, Grade B)
and marital satisfaction. Use OAB-q, OAB-S, OABSS, II-Q, or UDI (Grade A)
• OAB symptoms are linked to depressive illness (LoE 3b, Grade C).
• Individuals who develop UI have worse QoL. Self-completed voiding diary (LoE 2b, Grade B)
• OAB remains a serious concern in frail or multimorbid older people, although Document the time, type, and volume of fluid intake, urine volume voided,
evidence on the psychosocial impact of OAB in this population is limited. urgency episodes, and incontinence episodes over 3-7 days
Urinalysis (LoE 3b, Grade C)
Diagnosis Perform in the initial evaluation of patients suspected of OAB
Initial assessment includes a history and physical examination, patient self-completed
QoL questionnaire, voiding diary observation for 3-7 days, and urinalysis (see Figure). Additional tests: Post-void residual volume (LoE 3b, Grade B);
Additional tests are indicated when the diagnosis remains uncertain after history and bladder/renal ultrasound (LoE 4, Grade C); cystoscopy (Grade C);
physical examination, when the symptoms do not correlate with physical findings, or CT/MRI (Grade C); UDS (LoE 1b, Grade A)
after failed previous treatment (Expert opinion).
Abbreviations: CT: computed tomography; II-Q: Incontinence Impact Questionnaire; LoE: level of evidence; MRI: magnetic resonance imaging; OAB-q: Overactive Bladder Questionnaire; OAB-S: Overactive
Bladder Satisfaction Questionnaire; OABSS: Overactive Bladder Symptom Scores Questionnaire; QoL: quality of life; UDI: Urogenital Distress Inventory; UDS: urodynamic study; UI: urinary incontinence;
UTI: urinary tract infection. Reference: Corcos J, Przydacz M, Campeau L, et al. CUA guideline on adult overactive bladder. Can Urol Assoc J 2017;11:E143-73. http://dx.doi.org/10.5489/cuaj.4586